Quantum AI Creates a Better Liquid Biopsy
June 24, 2025 -- A team led by researchers from the University of Chicago Pritzker School of Molecular Engineering (UChicago PME) has put Quantum Machine Learning (QML) on the job for early detection of cancer.
Their new technique, outlined in a recent paper in the journal Bioactive Materials, outperformed classical methods in distinguishing exosomes—microscopic particles exuded by cells—from cancer patients versus exosomes from healthy individuals, a potential revolution in cancer diagnosis.
“This is the first application of the Quantum ML on exosomes’ as well as nanoparticles’ biomechanical characteristics. Nobody has done this so far,” said first author Abhimanyu Thakur, who was with UChicago PME and the Ben May Department for Cancer Research during the research. “Traditionally, many different methods have been used to distinguish these particles, but those are time-consuming and tedious.”
Thakur, now with Harvard Medical School’s Department of Neurosurgery, conducted the research under renowned cancer expert, UChicago PME and Ben May Center Asst. Prof. Joyce Chen. Chen called the research “the first piece of the work” coming from her lab that fuses quantum machine learning and cancer research.
“In my lab, I always encourage the next-generation researchers to think about interdisciplinary approaches to do the research,” Chen said. “The traditional way is not the only way to solve these problems. This combined methodology can often solve these big problems better.”
Peers in the field said this is a better way to detect cancer “long before symptoms appear or a lump shows up on a scan.”
“By training a quantum-inspired algorithm to spot subtle electrical ‘fingerprints’ of nanoparticles and exosomes in a blood sample, the research team from UChicago shows a fast, label-free way to tell healthy cell vesicles from tumor-derived ones,” said University of Pennsylvania Presidential Associate Professor César de la Fuente, who was not involved with the research. “That means a clinician could potentially detect cancer earlier, and monitor it more frequently, without the time, cost, or invasiveness of a traditional biopsy.”
AI for health care
All cells produce exosomes, tiny particles that contain biological material like proteins, lipids and nucleic acids. But cancer cells release them in “tremendous amounts,” Thakur said. Although exosomes, like all extracellular vesicles, cannot reproduce like a cell, this glut of biological data provides researchers a powerful tool for cancer diagnosis.
“They mimic their parent cells,” Thakur said. “That's how exosomes have become a very important platform for liquid biopsy. Because they mimic their originating cells, they can be used to predict what is going on in the originating cells.”
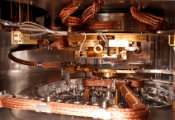
The “gold standard” for using these exosomes and other nanoparticles to detect cancer relies on transmission electron microscopes, massive machines that eat up lab space and cost upwards of $1 million, Thakur said.
The team took a novel approach to this problem. Instead of the complicated process of tagging, labeling and distinguishing which exosomes came from cancer cells and which came from healthy ones, the team looked at the particles’ electrokinetic attributes.
Co-author Asst. Prof. Jianpan Huang of the University of Hong Kong’s Department of Diagnostic Radiology helped design the algorithms to detect these subtle electrical signals.
Next steps
Beyond earlier, better cancer diagnosis, this new procedure opens up a wide variety of potential applications in biopharmaceutics, including pharmacokinetics (the study of what the body does to a drug) and pharmacodynamics (the study of what a drug does to the body).
Getting to this healthier future demands more data to help train and hone the machine learning algorithms.
“It is important to note that the current demonstration was conducted using a single dataset,” Huang said. “Future research involving datasets from multiple centers would be valuable to validate and strengthen these findings, as well as to further refine the methodology. Multi-center validation is essential for translating this technology into practical, real-world applications.”
This includes testing the process on different types of cancers.
“The hurdle is, biological systems are complex,” Chen said, “We have to adapt our algorithm and software to the real systems. For example, this research studied colorectal cancer. If you apply it to lung cancer or bladder cancer, that might not work very well. We need to retrain the machine before we are to continue to see promising results.”